What to engrave on your MedicAlert medical ID for ulcerative colitis:
MedicAlert offers free custom engraving on all our ulcerative colitis bracelets and medical ID products. Engravings on medical IDs for ulcerative colitis should include any critical medical information that can protect and save lives in an accident or medical emergency, for example:
- Ulcerative colitis
- NO NSAIDs
- Current medications
- Other medical information that needs to be communicated to first responders
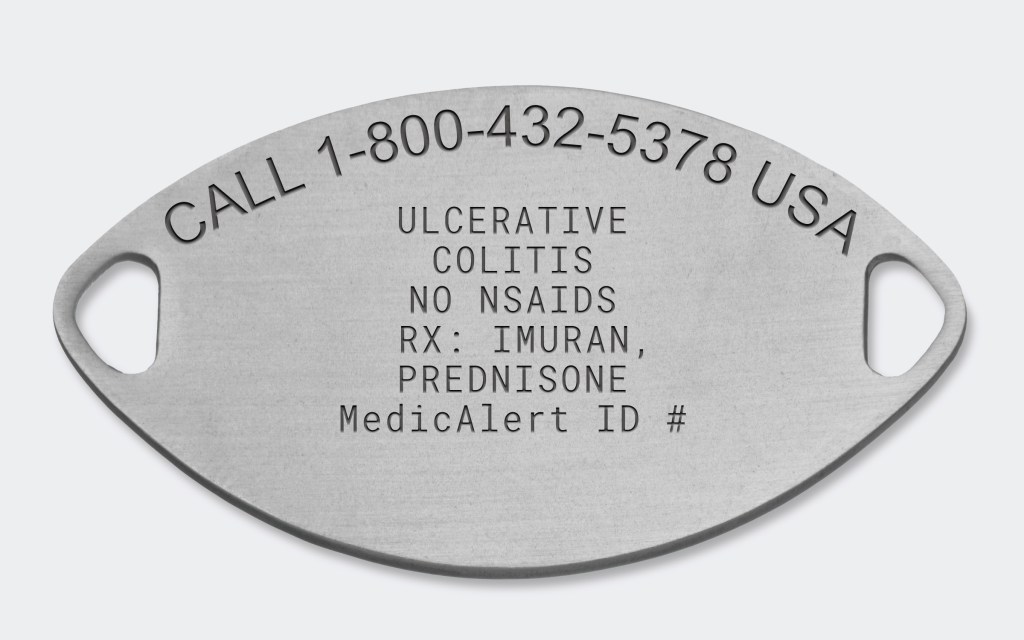
Sample engraving. Consult our team if you need help engraving your medical ID for ulcerative colitis.












