Like other boys his age, I’mere loves going to the park, eating spaghetti and fruit, and visiting Disneyland. Nothing stops I’mere from playing an energetic game of hide and seek or enjoying his Sonic toys, not even the seizures he withstands or the bleeding disorder Hemoglobinemia E (HbE). Hemoglobinemia E is an inherited...
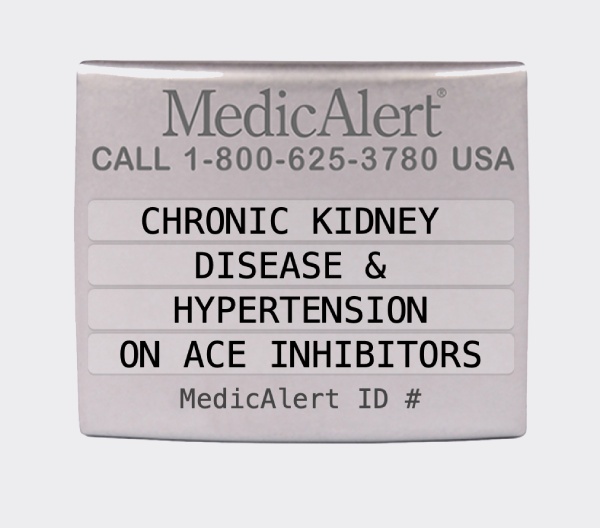
Medical-alert accessories, typically a bracelet, serve to transmit critical information about CKD to a health care provider, especially when the wearer is not able to reliably communicate.
National Institutes of Health