Be sure your loved ones have some form of identification on them, and keep in mind they may take off certain items of clothing or lose their wallets. Multiple forms of identification, emergency contact numbers and disclosure of their medical diagnosis of dementia are a good idea, including an ID bracelet or pendant, identification inside their clothing, and in their wallet.
AARP

Medical IDs for Demetia
Related Articles: Alzheimer’s Wandering
As of 2022 there are over 55 million people worldwide living with dementia, and 60% of them will wander from safety as a result. Learn how you can protect yourself and your loved ones with a MedicAlert ID and Safe & Found® Membership.
The confidence to live with dementia
Every 3 seconds someone in the world develops dementia. As of 2022 there are over 55 million people worldwide living with dementia. The WHO estimates this number will almost double every 20 years, reaching 78 million in 2030 and 139 million in 2050.
Another staggering statistic is that 6 out of 10 people with dementia will wander from safety. When someone with dementia wanders, they’re often unable to tell others where they live or how to contact their caregiver. If they aren’t located within a few hours, the odds of injury or death increase dramatically.
MedicAlert services drastically improve outcomes in wandering incidents with our 24/7 Safe & Found membership. Paired with an unremovable medical ID for dementia, MedicAlert keeps your loved one safe while providing you with enhanced peace of mind.
We are specialists in wandering safety. When a MedicAlert member is reported missing, it triggers our Safe and Found services. MedicAlert creates and distributes a bulletin to local law enforcement and hospitals, and coordinates with the family to ensure their loved on returns safely home. When your loved one wanders and can’t communicate, MedicAlert can be their voice.
Medical IDs for dementia are a way to empower your loved one and ensure they are safely returned home if they ever have a wandering incident.
How MedicAlert protects people with dementia
Living with dementia can be stressful. One thing you shouldn’t worry about is what could happen in an emergency. MedicAlert’s membership plans offer benefits that extend beyond the ID, providing safety and peace of mind for people living with dementia, their families and caregivers.

Safe & Found
If your loved one wanders, we’re here 24/7 to help ensure a safe return home.

Emergency Contact Notification
In an emergency, we connect families so that no one is alone in a crisis.

24/7 Emergency Response
Our team provides first responders the information they need to provide fast, accurate care.

Digital Health Profile
All your vital information, all in one place for you and your caregiver.
Pair a medical ID for dementia with a Safe & Found Membership.
What’s the difference between dementia and Alzheimer’s disease?
Dementia is a general term for conditions that have a group of symptoms including memory loss, cognitive decline, and impaired communication. Alzheimer’s is a specific type of dementia, and the most common type – accounting for 60-80% of cases.
Types of irreversible dementia:
Alzheimer’s disease
As the most common form of dementia, Alzheimer’s comprises 60 to 80 percent of dementia cases. Usually a slowly progressing disease, the average person lives four to eight years after receiving the diagnosis. Some people may live as long as more than 20 years after their diagnosis.
Alzheimer’s happens because of physical changes in the brain, including a buildup of certain proteins and nerve damage.
Dementia with Lewy bodies
Dementia with Lewy bodies is a form of dementia that occurs due to clumps of a protein in the cortex. In addition to confusion and memory loss, dementia with Lewy bodies can also cause:
- imbalance
- sleep disturbances
- hallucination
- other movement difficulties
Vascular dementia
Vascular dementia, also known as multi-infarct or post-stroke dementia, accounts for approximately 10 percent of all cases of dementia. It’s caused by blocked blood vessels. These occur in strokes and other brain injuries.
Parkinson’s disease
Parkinson’s disease is a neurodegenerative condition. In its later stages Parkinson’s can produce symptoms similar to Alzheimer’s. The disease more commonly leads to problems with movement and motor control, but it also can cause dementia in some people.
Frontotemporal dementia
Frontotemporal dementia is a group of dementias that often cause changes in behavior and personality. It can also cause language difficulty. Frontotemporal dementia can occur due to a variety of medical issues, including Pick’s disease and progressive supranuclear palsy.
Mixed dementia
When multiple types of dementia-causing brain abnormalities are present, this is sometimes referred to as mixed dementia. Most commonly this is Alzheimer’s and vascular dementia, but can include other forms of dementia as well.
Types of reversible dementia:
Delerium
Particularly in the older population, fevers and infections can cause delirium, a state of extreme disorientation that can be easily confused with dementia because it shows many of the same symptoms. The onset of delirium is noticeably more sudden than dementia and can worsen or improve drastically in a matter of hours or days. Delirium is not caused by gradual damage to the brain but rather by external factors like infections, strokes, withdrawal, or adverse reactions to medications.
Normal Pressure Hydrocephalus
Caused by a build-up of excess cerebrospinal fluid in the ventricles of the brain, normal pressure hydrocephalus is a form of dementia. This fluid buildup causes ventricles to expand damages surrounding tissue, leading to to difficulty walking, loss of bladder control, as well as symptoms common to dementia like cognitive impairment and memory loss. Hydrocephalus can be treated and reversed by draining the excess fluid from the brain through the surgical implantation of a shunt.
The concrete cause of cerebrospinal fluid buildup hasn’t yet been identified, but cerebrovascular disease, Alzheimer’s disease, hypertension, and vascular disorders are thought to increase the risk of developing normal pressure hydrocephalus.
Subdural Hematomas
Subdural hematomas, or blood clots in the brain, are caused by bruising from severe head trauma. In older people blood clots can occur even as a result of very minor head injuries which may be unnoticed. Hematomas can actually cause dementia symptoms, though quickly treating and removing the blood clot can restore brain function.
Thyroid Disease
When the thyroid gland is overactive (or underactive) overall body functioning decreases, which can lead to dementia. Women are up to five times as likely as men to develop thyroid-related dementia. Thyroid supplements can eliminate thyroid-related dementia symptoms and fully restore functioning, yet consistent medication and life-long treatment are needed to manage thyroid disease.
Toxic Reactions to Drugs or Chemicals
Certain medications or interactions between medications can result in dementia. Some types of poisoning like carbon monoxide, lead, mercury, or other heavy metal poisoning can lead to dementia symptoms which will diminish once exposure is stopped.
Alcoholism (especially alcohol poisoning) and heavy drug use and can also lead to dementia symptoms that may decrease after the substance abuse is stopped. However, with long-term or serious substance abuse permanent damage may occur, resulting in a condition known as substance-induced persisting dementia.
Tumors
Though it’s uncommon, tumors and cancers in certain parts of the brain can cause damage to surrounding tissues, causing dementia. Tumor-related dementia will usually be accompanied by severe symptoms like headaches, vomiting, or sudden personality changes. Treating or removing such tumors will cause dementia symptoms to significantly reduce if not disappear altogether.
Vitamin B12 Deficiency
Along with iron, vitamin B12 aids in the production of red blood cells, so vitamin B12 deficiency can contribute to dementia caused by pernicious anemia. Symptoms of pernicious anemia include fatigue, yellowed skin, pica, and shortness of breath along with dementia symptoms like confusion and difficulty concentrating. Usually, pernicious anemia is caused by an inability to properly absorb and retain the vitamin, not by a lack of vitamin B in the diet or dietary issues.
Pernicious anemia is sometimes genetic, through it more frequently results from weakened stomach lining (atrophic gastritis) or autoimmune conditions. Vitamin B12 supplementation can reverse pernicious anemia, as well as the dementia symptoms that accompany it. However, medications must be taken consistently to prevent the onset of dementia symptoms, as pernicious anemia is not completely curable.
Wernicke-Korsakoff Syndrome
Wernicke-Korsakoff Syndrome is a type of dementia caused by chronic, long-term alcoholism which leads to thiamine (vitamin B1) deficiencies. Thiamine converts sugar to energy for brain cells, so if thiamine levels are low the brain becomes unable to function properly. It’s unclear why alcoholism leads to thiamine deficiency in some alcoholics and not others, though poor nutrition is often cited as a likely main factor.
Though abstinence can restore memory and cognitive functioning to some extent, Wernicke-Korsakoff syndrome is only partially reversible. The condition causes permanent damage to the brain that cannot be reversed even upon discontinuing alcohol use.
What causes dementia?
Dementia occurs due to physical changes in the brain. It is generally caused by damage to or disruptions of brain cells, particularly in the cerebral cortex (the part of the brain which controls consciousness, memory, perception, and language). In some cases this damage or disruption isn’t permanent, causing reversible dementia conditions that can be slowed or cured with proper treatment.
Except for cases of reversible dementia, it is considered a progressive disease, which means it gets worse over time. For some people dementia progresses rapidly, while it may take years to reach an advanced stage for others. The progression of dementia depends greatly on the underlying cause. While people will experience the phases of dementia differently, most people with dementia share some of the symptoms.
Caring for someone with dementia
If in-home health aides cannot come by as frequently, family members and other caregivers may need to take on more caregiving responsibilities.
You can prepare for unexpected gaps in care by first making a list of essential supplies, such as medication, food, and personal hygiene products.
You should also research adult day care programs that could be useful if regular caregivers are not available.
It can be very helpful to establish a consistent daily routine that includes activities such as:
- set times for waking up and going to sleep
- bathing, dressing, and other personal care activities
- preparing and eating meals
- napping or resting
- relaxing or creative activities
- gentle physical activity
- socializing with friends and family
Minimizing stress is especially important for those living with dementia. For instance, if the person becomes withdrawn, frustrated, or confused it is helpful to find which activities are most soothing to the person.
It helps to create a calming atmosphere by keeping the person’s environment lit with soft warm lighting rather than harsh unnatural light, and to provide a relaxing sound experience by reducing loud noises and providing a variety of silence, interaction and relaxing music and/or natural soundscapes.
If someone with dementia becomes angry or upset, provide calm reassurance and ask them what they need, or what will help them feel comfortable.
If talking with the person does not help, caregivers can try redirecting the situation. For example, they might suggest a different activity or ask the person whether they want to move to another space in the home.
People with dementia may require additional support and visual cues to help them remember essential routines like hygiene practices. Caregivers may wish to practice thorough hand washing with the person.
Additionally, an alcohol-based hand sanitizer can be placed in an easily accessible place to encourage good hygiene, which can be especially helpful during flu season or Covid outbreaks.
People living with dementia cannot always communicate their needs to others. As a result, caregivers should regularly inquire about physical comfort and known issues, as well as evaluate the person’s physical health. Alert a physician if you notice changes in weight, appetite, bathroom habits, or increased confusion or agitation.
Engraving your MedicAlert ID for dementia:
- Dementia
- Name of person wearing ID
- Who to contact if wandering
- Any other significant medical conditions or medications
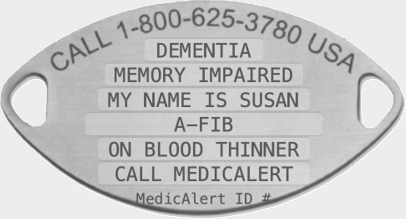
Sample engraving. Consult our team if you need help engraving your medical ID for dementia.
Find your medical ID.
Most appropriate types of medical IDs for dementia
For those with dementia it is best practice to apply a swiss cheese approach with medical IDs, meaning the more layers of protection, the better. For example, you might pair a bracelet for dementia with a bright ID tag and an ID sticker on the person’s mobility device. Bright colors can be especially useful for helping others identify a less traditional medical ID tag.
While many folks with dementia are fine with wearing a medical ID bracelet, jewelry is not for everyone. Some elderly adults with dementia or other cognitive challenges have a problem with an ever-present bracelet. Though for those who tolerate a bracelet, unremovable medical IDs for dementia can be a good way to make sure the ID is not removed, during a wandering incident for example.
Non-removable IDs for dementia have intentionally difficult-to-open clasps (such as a sister hook) that require 2 hands to open, such as recommended by Alzheimer’s organizations. To make the bracelet more difficult to remove, it can be placed on the person’s writing hand.
A common question is: Does my loved one need a medical ID if they have a tracking device? Yes, the more layers of identification, the better. Additionally, pairing IDs and tracking devices with a MedicAlert Protection Plan that includes Safe and Found services offers another layer of protection in incidents where wandering occurs.
Beyond bracelets, there’s a world of other options for medical IDs. The list of options for medical IDs for dementia continues to expand as technology advances. Whereas traditional IDs are wearable jewelry, such as bracelets and necklaces, there are clever alternatives such as Smart ID shoe tags, stickers and more.
Here are some alternative Medical IDs for dementia:
Smart IDs bring medical IDs into the digital age. MedicAlert’s Smart IDs are available as either Smart Medical ID Cards or MedicAlert ICE Tags. Both options use proven QR code technology for fast, easy access to your full health profile. Scanning the unique QR code on either type of Smart ID with a smartphone camera opens up critical information, including medical conditions, allergies, medications, vaccinations, and more. Since the QR code stores your data, you can fit more on one tag or ID, which can help with choosing a less obtrusive Smart ID or tag. Also, with Smart IDs your data can be updated without purchasing a new physical medical ID.
MedicAlert’s Smart Medical ID Card is credit card-sized and easily carried with you in a wallet or pocket. MedicAlert ICE Tags come in a set of four durable vinyl stickers that adhere securely to any hard surface – think cellphone cases, mobility aids – typical objects that travel with you. Each set of four tags has a unique QR code for one person, so they can be attached to multiple objects. Additional users would need their own individual set of sticker tags.
The portability and scope of personal medical information they provide make Smart IDs a great alternative to traditional jewelry and wearable IDs, not just in emergency situations, but also for doctor visits, home healthcare providers, or for access by other caregivers. Because they are digitally linked to your MedicAlert full profile, your information is automatically updated with any changes to your profile.
Apple Watches have become popular among all age groups. They are such an easily-accessible resource for all kinds of information, MedicAlert developed an ID specifically for Apple Watches. Although they are considered wearable, these attachable tags slide onto the silicone band of an Apple Watch, so they don’t require the addition of an entirely new piece of jewelry. The engravable tags are rust-proof, water-proof and made of stainless steel. They are available in multiple colors and several size options for compatibility with different sizes of Apple Watches.
Medical ID necklaces can range from utilitarian to fashion-forward, with several style options for children, women, and men. Like bracelets, necklaces can be made from a number of different materials or combinations of materials, such as stainless steel, sterling silver, gold, or platinum. MedicAlert necklaces come in a variety of chain and emblem styles, and also offer different color options for the engraving.
These types of medical IDs for Alzheimer’s can be perfect for individuals for whom any wearable ID is not a good option, such as seniors with strength limitations or cognitive issues. MedicAlert Shoe Tags are engravable and available in two different designs for easy and secure attachment to lace-up and other types of shoes.
If digital tech is too high-tech for the user, MedicAlert Fillable Wallet Cards are the manual alternative. Personal medical information and MedicAlert ID numbers are written by the owner or caregiver into the foldable card and must be physically updated when information changes. Like Smart ID cards, Fillable Wallet Cards are credit card-sized for portability, but unlike Smart IDs, the information is not digitally linked to a health profile.

MedicAlert Foundation and Alzheimer’s Association are long term collaborators in addressing the wandering crisis.
Living with dementia? Get peace of mind.
Pair your ID with a MedicAlert Membership.
If a person with dementia is in an accident or has a wandering episode, they can have difficulty communicating the details of their condition or other information important to their care. A MedicAlert medical ID for dementia lets emergency responders and ER doctors know that you are living with condition. A MedicAlert ID can also help your rescue team get in touch with loved ones and other emergency contacts.
When paired with a MedicAlert protection plan, our medical IDs become even more valuable in emergency and other medical situations. Our unique 24/7 Safe & Found program ensures your loved one is returned home swiftly and safely when they have a wandering incident.
Additionally, a MedicAlert protection plan can ensure accurate and fast care by providing detailed information about your condition, your full health profile, designated physician information, details about current treatment plans and any other conditions, and other vital information about your care. With a MedicAlert ID and protection plan, you will always have a voice in an emergency.

We'll be your voice. If you can’t communicate well enough to speak for yourself, your ID will speak for you, informing others about your dementia, major symptoms, and any medications you are taking.
We provide 24/7 emergency protection. Our team will relay your critical medical information to first responders in an emergency, no matter where or when it happens.
We keep you connected. You or a loved one should never have to be alone in an emergency. That’s why MedicAlert will reach out to your emergency contacts when needed if you are unable to do so.
We enable you to live with confidence. The freedom to live your life with dementia, knowing that MedicAlert is there for you.
Don't live in fear of wandering. With a Safe & Found Membership, you have 24/7 backup who will help you get home safely.
DISCLAIMER: THIS WEBSITE DOES NOT PROVIDE MEDICAL ADVICE. The information in this article is presented for educational purposes only and is not intended as a substitute for professional medical advice, diagnosis and treatment. Always seek the advice of a physician or other qualified healthcare provider for any questions you may have regarding a medical condition or treatment.



